Complete Guide to Diagnosis and Treatment of Hypertension

Hypertension, commonly known as high blood pressure, affects millions of people worldwide and is a leading risk factor for cardiovascular diseases such as heart attack, stroke, and kidney failure. Because hypertension often develops without noticeable symptoms, many individuals may live with it undiagnosed for years. Early detection and appropriate management are critical for reducing long-term health risks. Experts suggest regular blood pressure monitoring, lifestyle changes, and individualised medical care to maintain healthy blood pressure levels and prevent severe complications.
What Is Hypertension?
Hypertension refers to the condition in which the force of blood against the walls of the arteries remains consistently too high. Blood pressure readings are expressed with two numbers: systolic pressure (the top number, indicating pressure during heartbeats) and diastolic pressure (the bottom number, indicating pressure between heartbeats). A sustained reading of 130/80 mm Hg or higher generally indicates hypertension.
High Systolic vs. High Diastolic Blood Pressure
In many cases of hypertension, both the systolic (top number) and diastolic (bottom number) are elevated. However, some people may have high blood pressure affecting only one of these numbers. Healthcare providers use specific terms to describe these situations.
Isolated Systolic Hypertension
Isolated systolic hypertension occurs when the systolic pressure is 130 mm Hg or higher, while the diastolic pressure remains below 80 mm Hg. This type of hypertension is more common in older adults and is often linked to age-related stiffening of the arteries. As arteries lose elasticity over time, systolic pressure tends to rise even when diastolic pressure stays normal.
Isolated Diastolic Hypertension
Isolated diastolic hypertension is diagnosed when the diastolic pressure is 80 mm Hg or higher, but the systolic pressure is below 130 mm Hg. This form is less common and is more frequently seen in younger adults. It may be associated with increased resistance in smaller blood vessels.
Diagnosis and Tests of Hypertension
Hypertension is diagnosed based on consistent blood pressure readings that are higher than normal. Blood pressure is measured using two numbers, the systolic pressure and the diastolic pressure
- Stage 1 hypertension is defined as a systolic reading between 130 and 139 mm Hg or a diastolic reading between 80 and 89 mm Hg.
- Stage 2 hypertension is more severe and occurs when the systolic pressure reaches 140 mm Hg or higher, or the diastolic pressure is 90 mm Hg or higher.
Healthcare providers typically measure blood pressure during routine check-ups and other medical visits. A diagnosis of hypertension is made when elevated readings are recorded on two separate visits, with at least two measurements taken during each visit.
In addition to these stages, healthcare providers may use other blood pressure categories to guide treatment decisions:
- Elevated Blood Pressure: Blood pressure readings that are slightly above normal but not yet high enough to be classified as hypertension.
- Severe Hypertension: Extremely high blood pressure levels that have not yet caused organ damage but require urgent medical attention.
- Hypertensive Emergency: A critical condition in which dangerously high blood pressure is actively damaging organs such as the heart, brain, or kidneys. This condition causes noticeable symptoms and is considered a medical emergency requiring immediate care.
Management and Treatment of High Blood Pressure
The goal of hypertension treatment is to lower blood pressure to a safe range and reduce the risk of complications such as heart disease, stroke, and kidney damage. Treatment for hypertension typically involves a combination of medications and lifestyle changes. The goal is to lower blood pressure and reduce the risk of heart disease, stroke, and other complications. Common medications used to manage high blood pressure include:
- Diuretics
- Beta-blockers
- Calcium channel blockers
- ACE inhibitors
- Angiotensin II receptor blockers (ARBs)
The Role of Lifestyle Changes
Lifestyle modifications are a crucial part of blood pressure management for everyone, including those who are taking medication. In some cases, doctors may recommend lifestyle changes first before starting medication, depending on an individual’s health history and cardiovascular risk. Below are some effective lifestyle changes to lower blood pressure:
- Maintain a healthy weight
- Follow a nutritious eating plan
- Reduce sodium intake
- Increase potassium intake
- Stay physically active
- Quit smoking
- Limit alcohol consumption
The Bottom Line
Hypertension is a potentially dangerous condition that often goes unnoticed without regular monitoring. However, with accurate diagnosis, evidence-based treatment strategies, and continuous lifestyle management, high blood pressure can be effectively controlled.
Early and proactive care reduces the risk of complications and helps individuals lead healthier, stress-free lives. Access to experienced healthcare professionals and advanced care facilities, such as physicians available at top hospitals in Dubai, can further support accurate diagnosis, effective treatment, and ongoing blood pressure control.

 5 Toronto Dietitian Approved Habits for a Healthy New Year
5 Toronto Dietitian Approved Habits for a Healthy New Year  What Causes Gas And Bloating In Children?
What Causes Gas And Bloating In Children?  The Quiet Factors That Define a Reliable Angiography Device
The Quiet Factors That Define a Reliable Angiography Device  Renting medical equipment can make moving around and being comfortable easier
Renting medical equipment can make moving around and being comfortable easier  Finding the Best ObGyn Near Me: What Every Woman Should Know
Finding the Best ObGyn Near Me: What Every Woman Should Know 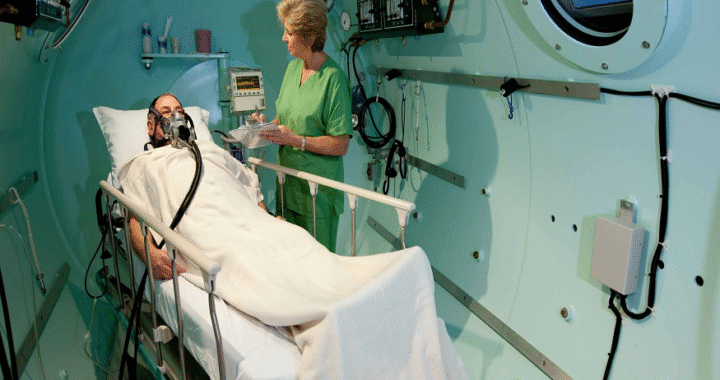 Repairing the Body with Hyperbaric Oxygen Therapy
Repairing the Body with Hyperbaric Oxygen Therapy  Complete Guide to Diagnosis and Treatment of Hypertension
Complete Guide to Diagnosis and Treatment of Hypertension  Moisturizer To Sheet Masks: Skincare Essentials To Pack For Colder Months
Moisturizer To Sheet Masks: Skincare Essentials To Pack For Colder Months  The Step by Step Process of Getting Dental Implants in Fargo
The Step by Step Process of Getting Dental Implants in Fargo