Key Breast Cancer Biomarkers: A Comprehensive Guide
Physicians use biomarkers to detect cancer early, when it is most treatable, and to understand the progression of the disease once it is established. Biomarkers are biological molecules that act as a signature for disease, indicating the presence and progression of cancer. This information can be used to guide both prognosis and treatment strategies. Understanding the significance of these biomarkers can help patients and healthcare providers make more informed decisions about their health and their patients’.
Understanding Breast Cancer Biomarkers
Biomarkers are biological molecules found in blood, other body fluids, or tissues that indicate a normal or abnormal process, linked to aspecific condition or disease. In the context of breast cancer, biomarkers are reveal valuable information about the cancer’s characteristics and behavior.
Biomarkers are vital in breast cancer care as they help in diagnosing the disease, predicting its progression, and determining the most effective treatment options. They enable personalized treatment plans, leading to better outcomes for patients.
Types of Biomarkers
Biomarkers can be categorized into three main types:
- Prognostic biomarkers: Indicate the likely course of the disease.
- Predictive biomarkers: Predict how well a patient will respond to a particular treatment.
- Diagnostic biomarkers: Help in identifying the presence of cancer.
Commonly Used Breast Cancer Biomarkers
Understanding the most commonly used breast cancer biomarkers is essential for grasping how they influence diagnosis, treatment decisions, and patient outcomes.
Estrogen Receptor (ER)
The estrogen receptor is a protein that, when bound by estrogen, can promote the growth of some breast cancers. ER-positive cancers rely on estrogen to grow.
ER status is determined through a biopsy where the tissue is tested to see if it has estrogen receptors. The presence of these receptors indicates an ER-positive breast cancer.
ER-positive breast cancers often respond well to hormone therapies that lower estrogen levels or block estrogen receptors, thereby inhibiting cancer growth.
Progesterone Receptor (PR)
Similar to the estrogen receptor, the progesterone receptor is another protein that can promote breast cancer growth when bound by progesterone.
PR status is tested alongside ER status. Both receptors are typically checked because their presence can influence treatment decisions.
PR-positive cancers also respond to hormone therapies, and knowing the PR status helps refine treatment plans, often in conjunction with ER status.
Human Epidermal Growth Factor Receptor 2 (HER2)
HER2 is a protein that promotes cell growth. In some breast cancers, an excess of HER2 protein leads to uncontrolled growth.
HER2 status is determined through tests such as immunohistochemistry (IHC) or fluorescence in situ hybridization (FISH).
HER2-positive breast cancers can be treated with targeted therapies that specifically inhibit the HER2 protein, slowing or stopping cancer growth.
Emerging Breast Cancer Biomarkers
Emerging and less common breast cancer biomarkers offer new avenues for understanding and treating complex disease, providingnew possibilities for personalized and effective therapies.
Ki-67
Ki-67 is a protein associated with cell proliferation. High levels of this protein indicate rapid cancer cell growth. Ki-67 levels are measured in biopsy samples to assess how quickly the cancer cells are dividing.
High levels can suggest a more aggressive cancer, helping doctors tailor more intensive treatment plans.
BRCA1 and BRCA2
Mutations in the BRCA1 and BRCA2 genes greatly elevate the risk of breast cancer. Normally, these genes assist in repairing DNA damage, and when they fail to function properly, cancer can develop. Genetic testing can detect BRCA1 and BRCA2 mutations, offering valuable information about hereditary cancer risk.
Knowing one’s BRCA status can guide preventative measures and treatment options, including more aggressive surveillance or preventive surgeries.
PD-L1
PD-L1 is a protein that can suppress the immune response, allowing cancer cells to evade detection. These levels are assessed to determine the potential effectiveness of immunotherapy treatments.
High PD-L1 levels can indicate that a patient might benefit from immunotherapies designed to boost the immune system’s ability to fight cancer.
Biomarker Testing Methods
Biomarker testing methods are crucial for accurately identifying and understanding the specific characteristics of breast cancer, guiding diagnosis and treatment decisions.
Immunohistochemistry (IHC)
IHC involves staining tissue samples with antibodies that bind to specific proteins, making them visible under a microscope. IHC is commonly used to test for ER, PR, and HER2 status, helping to classify the cancer and guide treatment.
Fluorescence In Situ Hybridization (FISH)
FISH uses fluorescent probes to bind to specific DNA sequences in the tissue, allowing visualization of gene abnormalities.
FISH is often used for HER2 testing when IHC results are ambiguous, providing a more detailed analysis of gene amplification.
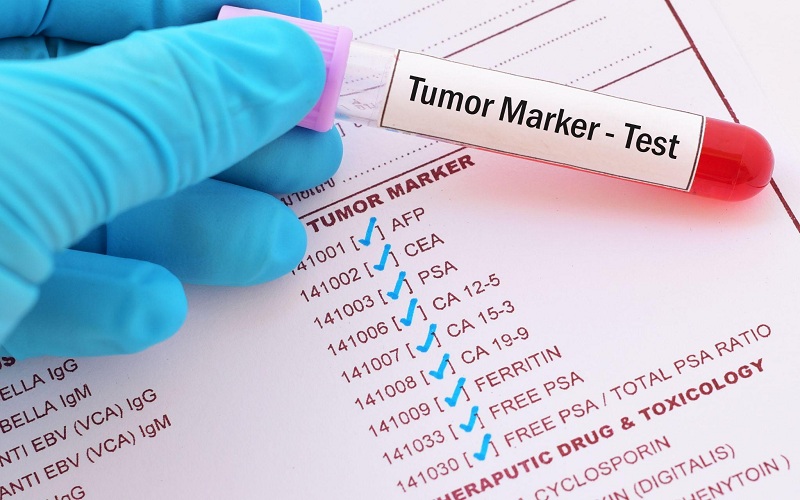
Tumor Marker Test
A tumor marker test measures the presence of specific proteins or genes in the blood, urine, or tissues that are associated with cancer.
These tests can help detect the presence of cancer, monitor the progress of the disease, and evaluate the effectiveness of treatment. Tumor marker tests are valuable in ongoing cancer management and can provide early indications of recurrence.
The Role of Biomarkers in Personalized Medicine
Biomarkers enable precision medicine by allowing treatments to be tailored to the specific characteristics of a patient’s cancer. This approach improves treatment efficacy and reduces unnecessary side effects.
Biomarkers are also used to monitor how well a treatment is working. Changes in biomarker levels can indicate the effectiveness of a therapy or signal the need for adjustments.
Conclusion
Breast cancer biomarkers play a crucial role in the diagnosis, prognosis, and treatment of the disease. Understanding these biomarkers and their implications can empower patients and healthcare providers to make more informed decisions, leading to better outcomes. As research continues to advance, the hope is that biomarker-driven personalized medicine will become even more precise and accessible, improving outcomes in breast cancer care.

 Complete Guide to Diagnosis and Treatment of Hypertension
Complete Guide to Diagnosis and Treatment of Hypertension  5 Toronto Dietitian Approved Habits for a Healthy New Year
5 Toronto Dietitian Approved Habits for a Healthy New Year  What Causes Gas And Bloating In Children?
What Causes Gas And Bloating In Children?  The Quiet Factors That Define a Reliable Angiography Device
The Quiet Factors That Define a Reliable Angiography Device  Renting medical equipment can make moving around and being comfortable easier
Renting medical equipment can make moving around and being comfortable easier  Finding the Best ObGyn Near Me: What Every Woman Should Know
Finding the Best ObGyn Near Me: What Every Woman Should Know  Moisturizer To Sheet Masks: Skincare Essentials To Pack For Colder Months
Moisturizer To Sheet Masks: Skincare Essentials To Pack For Colder Months  The Step by Step Process of Getting Dental Implants in Fargo
The Step by Step Process of Getting Dental Implants in Fargo